Source: U.S. Renal Data Systems Quarterly Update
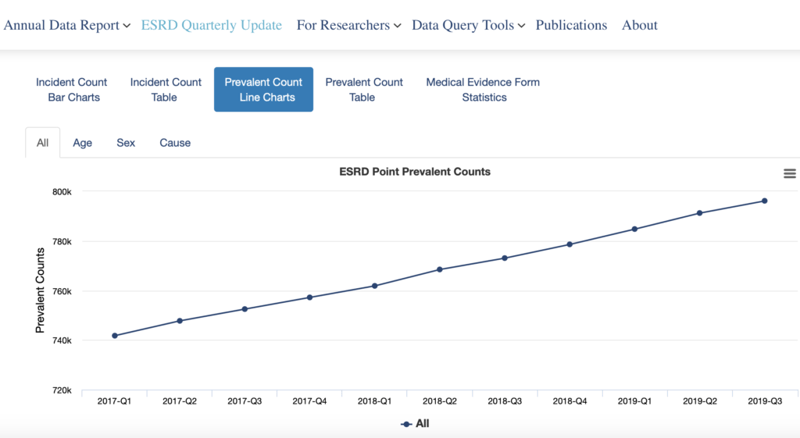
An alarming trend continues: the number of people living with end-stage renal disease (ESRD) has climbed by approximately 20,000 each year over the past decade. Based on this trajectory, the number is expected to surpass 800,000 this year.
This situation risks being exacerbated by the number of COVID-19 Acute Kidney Injury (AKI) survivors who developed renal failure while hospitalized and required emergency dialysis to survive. It’s well established that AKI increases the risk of developing kidney disease. In fact, 31% of people who develop AKI while hospitalized are diagnosed with kidney disease, the precursor to ESRD, within a year of being discharged.
ESRD remains one of the most costly and complex chronic conditions to treat, taking a tremendous toll on patients and their families, healthcare providers and the health plans that provide coverage. We can slow the trend of ESRD patients, improve care for those living with ESRD and better manage costs by taking these three steps.
1. Prioritize early detection. Currently, over 37 million people are living with chronic kidney disease (CKD) and nine out of ten are unaware of their condition. Many will be diagnosed when renal failure drives them into an ER and they “crash” into dialysis.
Early detection remains the most effective means of treating kidney disease. With clinically proven interventions, diet and lifestyle changes can be introduced early to prevent or delay progression to ESRD, the most serious stage of the disease which requires dialysis or a kidney transplant to survive.
By leveraging advanced technology — big data, artificial intelligence (AI), machine learning, and predictive analytics, coupled with clinical expertise and care management — those at risk can be identified sooner. Providing healthcare providers with actionable and clinically proven data and care recommendations ensures patients receive the care they need to slow progression and better manage their condition.
2. Educate, engage, and empower. Kidney disease doesn’t just happen. It develops slowly over time, and most patients come to a diagnosis from a pre-existing condition, such as diabetes or hypertension. In fact, these two “gateway” conditions account for two-thirds of kidney disease diagnoses. Improved understanding of kidney disease, risks and symptoms is important for everyone, and even more so for those living with diabetes and/or hypertension. It’s an important first step in empowering patients in their health, well-being and care.
Research shows that when patients are engaged in their healthcare, outcomes improve. They’re more likely to adhere to their treatment and medication regimens, monitor their health, self-advocate, and ask their healthcare team questions. When patients are actively involved in their care and knowledgeable about their condition, adverse medical events that can result in ER visits and unplanned hospitalizations can be avoided, along with the significant costs associated with these unplanned events.
Connecting patients to community-based services, such as transportation, mental health, and meals on wheels, can help overcome the barriers that often keep patients from accessing their healthcare needs. With COVID-19 forcing many medically vulnerable patients to remain home as much as possible, telehealth has become an important lifeline. The involvement of care management teams, including nurses and social workers, are instrumental in assessing and supporting a patient’s telehealth readiness, while helping them transition to virtual care so that critical connections to their healthcare team can be maintained. Patients who feel supported report better member experiences.
3. Bring treatment in-home. In the U.S., in-home dialysis remains an underutilized treatment modality for ESRD patients, despite it being as safe and effective as in-center dialysis. Currently, only 12% of patients receiving dialysis do so at home. For the appropriate patients, in-home dialysis can be life-altering and freeing. In-home dialysis is also a more cost-effective option to in-center dialysis, costing approximately 15% less per patient per year.
(In-home Dialysis: Better Outcomes, Patient Experience and Costs)
With advanced technology, clinical expertise, and compassionate care, ESRD management can make a difference. The first step is to identify appropriate patients for in-home dialysis through early identification and provider consultation. Machine learning and predictive analytics can be deployed to uncover those whose medical profiles match that of other ESRD patients who have successfully transitioned to in-home treatment. Providers and patients can also proactively engage in planning for in-home dialysis, including setting up the support and services needed to make in-home treatment a success.
In-home dialysis represents a tremendous opportunity to improve quality of care, outcomes, member experience and costs. Disrupting the in-center dialysis treatment paradigm will require a concerted effort to properly plan effective kidney care for all patients.
Healthmap Solutions is working with a number of large health plans to implement these steps. Our Kidney Health Management (KHM) program delivers great results by reducing total medical costs by 15% to 20% while driving in-home dialysis steerage by 40%, a number which continues to improve, compared to the national average of 12%. For more information visit healthmapsolutions.com
To stay current on issues and breaking news related to kidney health management and population health management, follow us on LinkedIn, Facebook and Twitter @healthmapcare, and sign up for direct alerts from Healthmap Solutions.
