Sickle Cell Disease and Kidney Health
Sickle cell disease (SCD) raises the risk of chronic kidney disease (CKD) in a population that is already significantly more likely to develop CKD—and less likely to receive equitable health care.
What is sickle cell disease?
SCD is a hereditary condition that affects approximately 100,000 people in the United States. Its most common and most severe form is sickle cell anemia.
SCD gets its name from the effect it has on red blood cells. Red blood cells contain hemoglobin, a protein that transports oxygen. Normally, red blood cells are round, smooth, and flexible, allowing them to move easily through small blood vessels to carry oxygen to all parts of the body. However, in someone with SCD, the hemoglobin is abnormal and causes the red blood cells to become hard, sticky, and crescent-shaped, like a farmer’s sickle.
As a result, sickle cells get stuck in smaller blood vessels, restricting the flow of blood and oxygen to parts of the body. This often causes severe pain and other serious complications.
What does SCD have to do with kidney disease?
Kidney injury and chronic kidney disease are potential complications of sickle cell disease. Since the kidneys are made up of millions of tiny blood vessels, they are especially sensitive to restricted blood flow. The lack of oxygen causes kidney cells to die and the organ to lose its ability to filter waste. According to Sickle-Cell.com:
“Chronic kidney disease is common in SCD and shows a range of conditions, called sickle cell nephropathy (SCN). Sickle cell nephropathy leads to chronic kidney disease in 1 out of every 3 to 4 adults with SCD. People with sickle cell anemia or sickle-beta0 thalassemia have a higher risk than people with other types of SCD. About 1 in 6 people with SCD die because of chronic kidney disease.”
Who is at risk for SCD?
SCD affects African Americans at much higher rates than people of other ethnicities. The Centers for Disease Control and Prevention (CDC) estimates that SCD occurs in one out of every 365 African American births. In 2021, the U.S. saw a little over 517,000 African American births. Using the CDC’s estimate, that would account for around 1,400 children born with SCD genes. Among African American patients, SCD (and to a lesser extent, sickle cell trait) was associated with a faster kidney function decline, according to study findings published in the Journal of the American Society of Nephrology.
SCD isn’t limited to African American populations. It also occurs in one out of every 16,300 Hispanic American births.
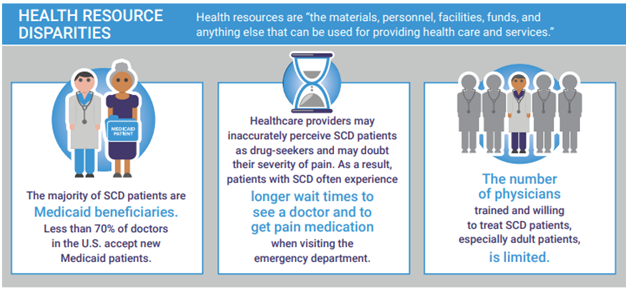
Thus, there is a higher risk of both SCD and CKD in racial and ethnic populations that are already disproportionately burdened by kidney failure and limited access to health care. The CDC Foundation points out that as a group, people with SCD have access to fewer health resources and experience worse health outcomes compared to other diseases, as shown in the infographic below.
End-stage renal disease (ESRD) will occur in one of every ten people with both SCD and CKD, but these individuals are less likely to be placed on a kidney transplant list than those without SCD. It is important to better understand why these barriers to transplantation exist (whether they are related to implicit biases, social barriers to care, or related medical conditions) so that people with both SCD and CKD have more equitable access to kidney transplants.
Our Executive Briefing, “Health Equity and Kidney Disease Management,” offers a deeper dive into healthcare inequalities.
What can be done?
With early diagnosis, a healthcare provider can recommend medicines to prevent sickling, reduce pain crises, reduce the risk of infection, and reduce or prevent complications.
Hydroxyurea, a medicine that helps red blood cells stay rounder and more flexible, is a mainstay in the overall treatment of children and adults with SCD since it reduces the frequency of pain crises and prolongs survival. Among those with CKD, angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs) are used to slow kidney damage and disease.
The doctor may also recommend a transfusion to treat and prevent certain complications of SCD. Transfusion options include:
- Acute transfusion to treat complications that cause severe anemia.
- Red blood cell transfusions to increase red blood cell count to normal levels.
- Regular or ongoing transfusions to reduce the risk of stroke in those who have already had an acute stroke.
Can SCD be cured?
Right now, the only FDA-approved therapy that may be able to cure SCD is a bone marrow or stem cell transplant. However, these are very risky procedures with potentially serious side effects, including death. For the transplant to be successful, the donor marrow must be a close match, usually from a sibling. While gene therapy is still under investigation, early studies using LentiGlobin for sickle cell disease have shown positive results in eliminating severe vaso-occlusive events.
How can Healthmap help?
SCD adds complexity to the management of CKD, a condition already likely to involve one or more comorbidities, and therefore places an even higher priority on communication and coordination between the primary care provider, nephrologist, and numerous specialists involved in a person’s care. Healthmap’s Kidney Health Management program provides the framework for such care integration through our Quality Practice Advisors.
As an organization with a passion for promoting health equity, Healthmap feels strongly that all kidney patients deserve to achieve their best possible health outcomes, regardless of their socioeconomic background. This is especially important for the populations that are at a higher risk of both SCD and CKD, as they commonly face systemic barriers to care. To combat these obstacles, our Care Navigators work directly with patients to provide the education they need to understand their condition and to help them overcome socioeconomic determinants of health and obtain access to quality care.
We Are Passionate about making a difference for patients with CKD and ESRD. We Are Healthmap!