It’s National Kidney Month!
March is National Kidney Month, a month dedicated to raising awareness of the vital need for proactive kidney healthcare. At Healthmap, that means working toward greater awareness among healthcare professionals as well as the general public.
Why is this so important?
- Approximately 37 million American adults have chronic kidney disease (CKD), and 9 out of 10 people don’t realize they have CKD.
- Among people with severely reduced kidney function, 40% are not aware of their CKD.
- Every 24 hours, 360 people begin dialysis treatment for kidney failure.
- Kidney diseases are a leading cause of death in the United States.
Source: CDC (Centers for Disease Control and Prevention)
Those are staggering numbers, but it doesn’t have to stay this way. Often, by making certain lifestyle modifications, CKD is both controllable and potentially preventable.
That’s why Healthmap works with primary care providers (PCPs) to sharpen their focus on:
- Educating patients about kidney health, with emphasis on the causes and effects of CKD
- Screening for early diagnoses of CKD, especially among patients already being treated for diabetes or high blood pressure
- Taking immediate steps to slow the disease’s progression
- Referring patients with CKD to a nephrologist at the earliest opportunity
This is also an appropriate time for practitioners to renew their own awareness and understanding of CKD, including the latest developments in treatment and management.
Kidney Basics
For a couple of small organs (about the size of one’s fist), the kidneys do a big job. Their primary function is to filter waste and excess water out of the bloodstream. The kidneys process blood to the tune of around 150 quarts a day. Given that the average adult body has 5 to 6 quarts of blood in total, a pair of healthy kidneys will filter the entire bloodstream approximately 30 times a day. That’s some heavy lifting!
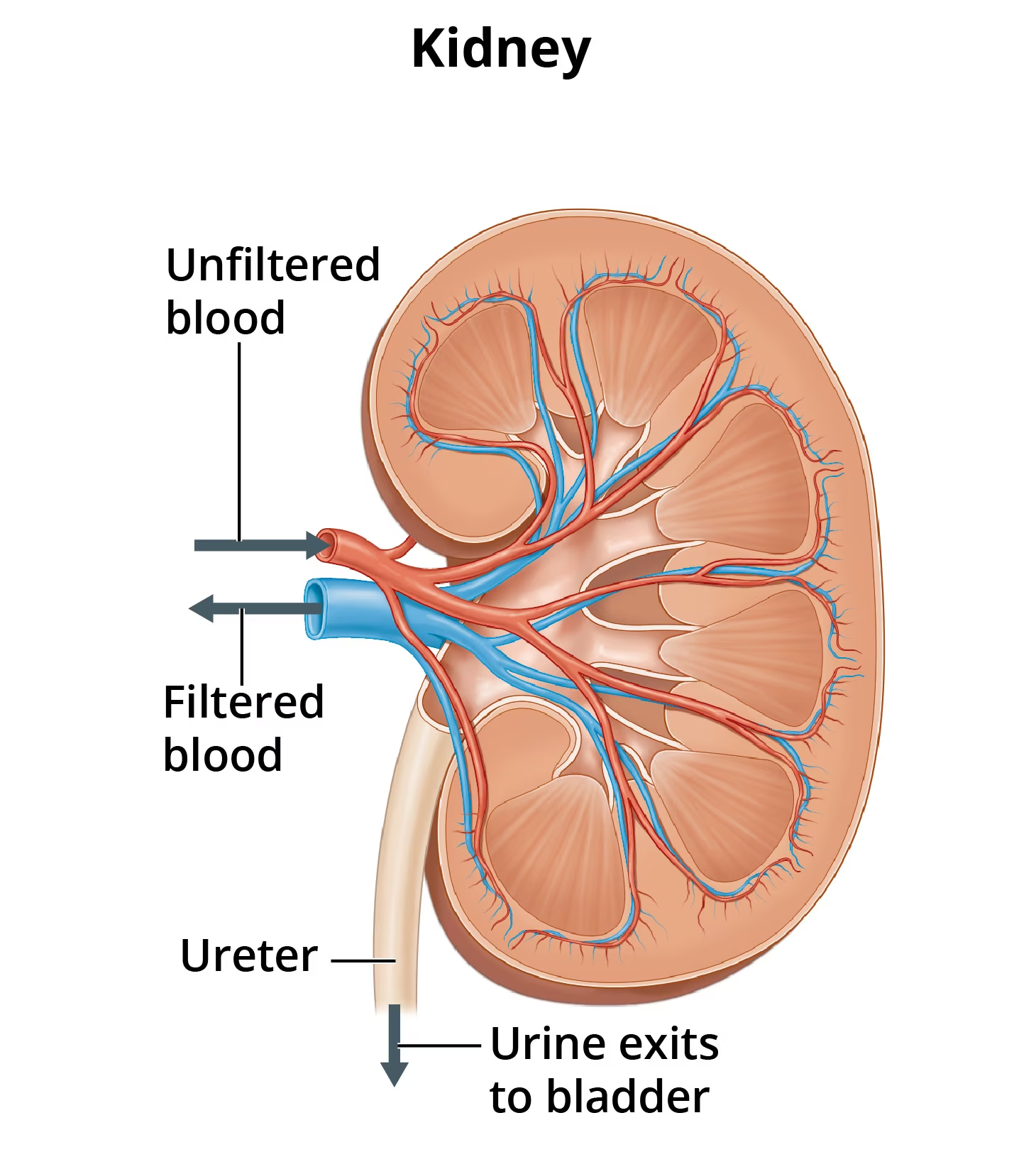
That’s not all. The kidneys maintain the proper balance of water, salts, and minerals in the body. They are also responsible for directing the production of red blood cells, regulating fluid, and controlling blood pressure.
Each kidney is made up of about a million filtering units called nephrons. Each nephron includes a filter, called the glomerulus, and a tubule. The glomerulus filters the blood while the tubule removes wastes and returns needed substances to the body via the bloodstream.
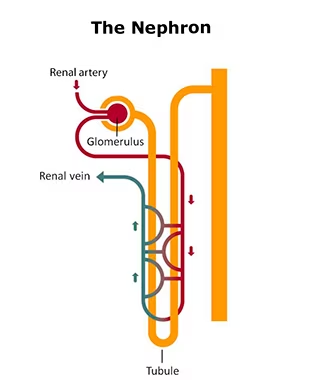
Images courtesy of the National Institute of Diabetes and Digestive and Kidney Diseases
For a more detailed explanation, see “Your Kidneys and How They Work.”
CKD Causes and Effects
The kidneys are delicate and can easily be injured by diseases like diabetes and high blood pressure. Over time, this injury leads to increasingly impaired function and eventual failure. The most common causes of CKD are in fact, diabetes and high blood pressure.
With diabetes, high blood glucose levels result in thickening of various membranes and blood vessels in the kidney which are required for healthy functioning. In addition, the kidney’s filtering system becomes damaged which leads to the loss of important proteins in the urine. With time, these changes lead to scarring within the kidneys which leads to irreversible loss of kidney function.
Similarly, high blood pressure damages blood vessels by causing them to become stiffer and thicker over time. When this happens, arteries become narrowed which makes it harder for blood to reach important organs (like the brain, eyes, heart, and kidneys). As a result, a person can not only develop kidney disease, but they are also at increased risk for heart disease and stroke.
According to the CDC, other consequences of CKD may include:
- Anemia, low red blood cell count
- Increased infections
- Low calcium, high potassium, and high phosphorus levels in the blood
- Loss of appetite
- Depression
Educating Patients
CKD, CVD, and type 2 diabetes all share similar risk factors including unhealthy diet, obesity, and unhealthy lifestyle (i.e., lack of exercise, smoking, alcohol/drug use). At Healthmap, our Care Navigation team (which consists of registered nurses with a specialization in kidney health) spends a lot of time educating patients about these preconditions. The reason is simple: if these preconditions can be controlled, then CKD can be slowed and better managed. In addition, we focus on helping patients understand:
- The essential role the kidneys play in body function and overall health.
- The inherent dangers of diabetes and heart disease as well as the concomitant risk of CKD.
- The changes they can make that will benefit their health now and over the long term.
We know that this is a tall order for PCPs, for whom time is in critically short supply. In the Healthmap Kidney Health Management (KHM) program, our Care Navigators extend a practice’s capabilities by working directly with CKD patients to help them understand their disease, adhere to their prescribed regimen, and actively engage in their own treatment.
For those not in the Healthmap KHM program, we suggest checking out the many patient-education resources available on the internet, starting with those available on the CDC’s Chronic Kidney Disease Initiative page.
Early CKD Diagnosis
Early CKD patient identification is the cornerstone on which Healthmap’s NCQA-accredited KHM program was built. Using advanced analytics, we scan patient data to identify those most at risk of CKD or who are already in the early stages. The earlier the intervention, the better the outcome.
This is important because, in its early stages, CKD is asymptomatic. Testing is the only way to know how well a patient’s kidneys are working. Providers should perform a blood test to establish the patient’s glomerular filtration rate (GFR), a measure of the kidney’s filtering efficiency, and a urine test to check for albumin, a protein that can pass into the urine when the kidneys are damaged. A GFR reading of 90 or more indicates normal function, while a reading below 90 may indicate kidney disease. A urine albumin (to creatinine ratio) result of 30 mg/g or less is normal, but more than that may be a sign of kidney disease.
Who should be tested? All individuals over the age of 60 should be given these tests on a regular basis (at least once a year). Priority should be given to those with known comorbidities (especially diabetes and high blood pressure) and to those with a family history of kidney disease. Anyone experiencing swelling, blood in the urine, excessive thirst, or fatigue should also be evaluated.
We can’t overemphasize: CKD screening is best done at the primary care level. When screening is done in a timely manner, we can avoid the all-too-common situation of patients receiving a diagnosis of CKD in an emergency setting, often while being treated for some other condition. In addition, this allows for providers to diagnose CKD early, with sufficient time to slow the disease’s progression and to help avoid renal replacement therapy (dialysis or transplant).
Now Is the Time
During National Kidney Month, we urge providers and patients alike to take time to:
- Learn the early, hidden symptoms of CKD
- Understand the health consequences of CKD
- Prioritize a healthy lifestyle (good diet, adequate exercise, cease smoking)
- Participate in timely screening for CKD
At Healthmap, we invite you to join us on our mission to spread kidney health awareness. Our number one priority is the health and well-being of the kidney patients we serve on behalf of our KHM program partners. We urge provider and payer organizations to put our advanced technology, superior clinical expertise, and complex care management know-how to work, to deliver improved care and superior patient outcomes. For more information on Healthmap’s services, contact us today.
We Are Leaders in delivering exceptional kidney care management. We Are Healthmap!